Project context and rationale
> The Bolobo Health Zone is made up of 23 health centres. Staffed by a doctor, the Nko Health Centre is the reference health centre, on which 5 others depend. It was constructed in 1945 at the intersection of two main roads (one connecting Mushie with Bolobo and one connecting Bolobo with Kinshasa via Lediba on the Kasai River). Currently, the Nko Health Centre serves 15 villages, 2 of which are in the Mushie Territory. Only two villages are considered to be close to the Nko Health Centre (the village of Nko, 1 km away, and the village of Nkala, 5 km away). The other villages are all located at a far greater distance, with the furthest being 25 km away.
> In the Nko Health Area, and the Bolobo Health Zone in general, the health situation is precarious, particularly the sexual and reproductive health situation, characterised by:
• a high number of maternal deaths and obstetric fistulas;
• a high number of births among minors (around 60%) with the
principal causes being forced and early marriages, and sexual violence;
• the precarious nature of technical platforms;
• the quality and insufficiency of healthcare personnel; and
• a lack of family planning.
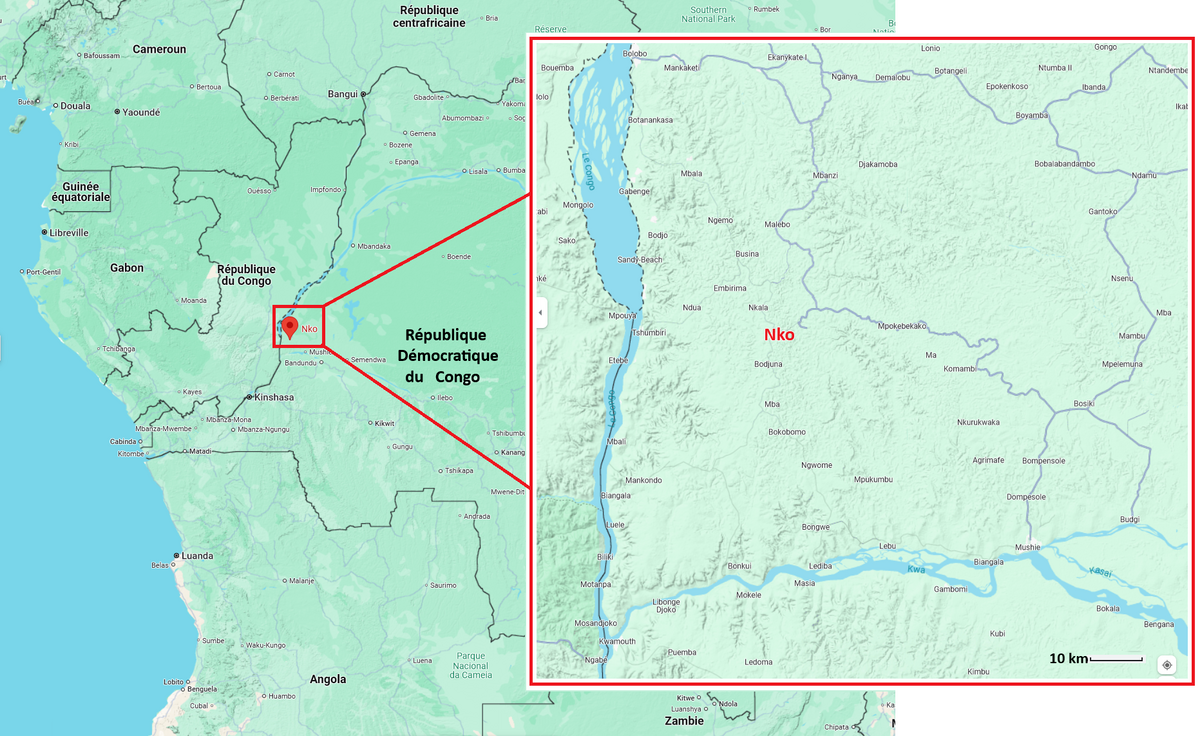
> It is important to note that in this region (see map below), whether in the immediate Nko Health Area or the wider surrounding area, there are no maternity wards or hospitals.

Map of Health Areas in the Bolobo Health Zone (DRC)té de Bolobo
> In view of the high number of maternal deaths recorded in the Nko Health Area and its surrounding areas, an alarm call was sounded by local communities and the region’s key figures, including the Chief Zone Medical Officer, the Provincial Medical Inspector, and the Provincial Minister for Public Health.
In response to this alarming situation, MMT was asked to intervene.
> Locally, the high number of maternal deaths is mainly due to:
- the precarious nature of the technical platform;
- the quality and insufficiency of healthcare personnel; and
- a low awareness of sexual and reproductive health, family planning, HIV/AIDS, and other opportunistic diseases.
> As a first step in helping these local communities – communities that are particularly invested in the protection of the forest, bonobos, and biodiversity in general – MMT has allocated all the funds received from the 2022 Ashden Prize to the construction of a new reference Maternity Clinic. However, the effective implementation and proper functioning of this new service will require the allocation of further funds.
Nature of the project
Setting up a maternity clinic in the Nko Health Area
(Bolobo Health Zone, Mai-Ndombe province)
> Improving maternal health in the region requires the identification and addressing of the barriers that limit access to quality maternal health services, both at health system and societal levels. As part of the Sustainable Development Goals (SDGs), SDG 3 has set an ambitious target:
"To reduce the global maternal mortality ratio (MMR) to less than 70 per 100,000 live births, with no maternal mortality ratio exceeding double the global average in any country.”
> Women die as a result of complications during and after pregnancy and childbirth. Most of the complications occur during pregnancy, and many of them could often be prevented or treated. Complications also occur before pregnancy and become worse during pregnancy, especially when not treated.
The 2020 global maternal mortality ratio was 223 per 100,000 live births.
According to the WHO, the main complications, responsible for nearly 75% of maternal deaths, are:
• severe haemorrhage (mainly after childbirth);
• infections (usually after childbirth);
• high blood pressure during pregnancy (pre-eclampsia, eclampsia);
• complications during childbirth; and
• unsafe abortion.
> The aim of this project is to contribute to the reduction of maternal and infant mortality in the Bolobo Health Zone.
|
Primary and secondary goals |
|---|
|
1. Improve pregnancy monitoring in the Nko Health Area |
|
2. Improve perinatal safety for mothers and children during childbirth in this area. |
|
3. Promote sexual and reproductive health in the Bolobo Health Zone. |
|
4. Assure the coordination of sexual and reproductive health activities in the Bolobo Health Zone. |
Methodology
> The various components required for the implementation of the project are as follows:
- Meeting with Technical and Financial Partners (TFP);
- Working sessions with the Health Zone Office to create a Steering Committee;
- Recruitment of project leaders;
- Planning, purchase, and procurement of necessary maternity and administration materials and equipment (see list of requirements below);
- Capacity building for project leaders;
- Project launch ceremony; and
- Implementation of project activities.
Framework of activities & implementation strategy in the Bolobo Health Zone
A - Promoting sexual and reproductive health in the community
|
Activities |
Implementation Strategy |
|
Capacity building of community actors in sexual and reproductive health, and innovative approaches to SRH |
Organise training sessions/workshops for community stakeholders (midwives, community relays, nurses, and doctors) on all contraceptive methods In collaboration with the zone health team, we will provide a number of innovative approaches to SRH, particularly regarding the use of recent contraceptive methods, including implants and 24-hour pills |
|
Raising awareness among women, men, and young people on HIV/STIs/FP/GBV |
Organise awareness days with women, men, and young people, screening videos about HIV/STIs/FP/GBV |
|
Distribution of contraceptive supplies |
Make ad hoc requests to UNFPA, FSS, DKT, and other partners for the provision of contraceptive supplies |
B - Strengthening support for the Nko / MMT maternity unit
|
Activities |
Implementation Strategy |
|
Capacity building of health service providers (midwives, nurses, and doctors) on SRH |
Organise a training workshop for healthcare service providers in collaboration with the zone health team on SRH |
|
Training of other healthcare providers (nurses, midwives) on SRH |
Organise a training workshop for healthcare service providers in collaboration with the zone health team |
C - Coordinating sexual and reproductive healthcare activities
|
Activities |
Implementation Strategy |
|
Steering Committee data analysis meetings |
Organise 4 Steering Committee meetings per year for data analysis purposes, bringing together service providers and partners |
|
Quarterly supervision missions with the zone health management team |
Quarterly supervision missions with the zone health management team |
|
Project surveys |
Plan and carry out 2 surveys |
Monitoring and evaluation
> With regard to information management, data collection tools will be provided for the two groups working in the field, being: (i) healthcare providers; (ii) community providers.
- Health care providers: will collect data at a health centre level and pass it on to be examined by DSH2 in order to follow the health pyramid, and also entered into the MMT database to ensure monitoring and advocacy based on the results.
- Community providers: will be trained in field data collection techniques. They will pass the data they collect on to their supervisors each month, where it will be sent on to the Health Zone in order to follow the health pyramid, and also entered into the MMT database to ensure monitoring and advocacy based on the results.
List of health indicators to be used to monitor individual health status
Consultations / Births Activities
|
Chapters |
Indicators |
|
Family |
• Number of monthly consultations in the Health Area |
|
Prenatal |
• Number of pregnancies being monitored |
|
Postpartum |
• Number of postpartum women being followed ups |
|
Childbirths |
• Number of deliveries |
|
Maternal, neonatal, |
• Number of maternal deaths: |
Patient Characteristics
|
Chapters |
Indicators |
| Physical characteristics |
• Age • Height • Weight • Nutritional status |
| Medical history |
• Congenital diseases • Acquired chronic diseases • Number of pregnancies (full term/interrupted) • Diseases/parasitoses identified |
| Socio-economic characteristics |
• Occupation (housekeeper, farmer, etc.) • Marital status (married, single, widowed) • Single parent, supportive or conflictual • Limited income • Access to drinking/non-drinking water • Access to shared/private toilets |
Budget forecast
Financial requirements for equipping the maternity clinic
|
No. |
Designation |
Qty |
Unit |
Total |
|
01 |
Solar system or lighting |
- |
3.315 US$ |
3.315 US$ |
|
02 |
Construction of toilets and showers |
- |
2.100 US$ |
2.100 US$ |
|
03 |
Baby hospital beds |
20 |
100 US$ |
2.000 US$ |
|
04 |
Adult hospital beds |
20 |
150 US$ |
3.000 US$ |
|
05 |
Surgical lamp |
1 |
250 US$ |
250 US$ |
|
06 |
Sterilisation autoclave, |
1 |
1.500 US$ |
1.500 US$ |
07 |
Mechanical or electronic baby scales |
1 |
58 US$ |
58 US$ |
|
Adult scale |
1 |
2.500 US$ |
2.500 US$ |
|
|
08 |
Medical consumables |
- |
1.500 US$ |
1.500 US$ |
|
No. |
Designation |
Qty |
Unit |
Total |
|
09 |
Ultrasound device |
1 |
4 500 US$ |
4 500 US$ |
|
10 |
Boxes: |
- |
1 000 US$ |
1 000 US$ |
|
11 |
Delivery table |
1 |
2 500 US$ |
2 500 US$ |
Total cost : 22.873 US$
Project financing status
Last updated: 10/31/2024


